Chronic granulomatous disease (CGD) presents with life-threatening infections caused by a hereditary defect in forming reactive oxygen. A retrospective case review conducted at the Instituto Nacional de Salud del Niño (INSN), Breña, over the last 10 years allows us to understand the demographic, laboratory, and clinical characteristics of affected patients within a Peruvian pediatric population.
To describe clinical manifestations and laboratory findings of eight children with CGD.
Demographic characteristics
| Patients . | Sex . | Symptom onset (months) . | Age at diagnosis . | Current age . |
|---|---|---|---|---|
| P1 | Male | 6 | 2 years | - |
| P2 | Male | 2 | 6 months | - |
| P3 | Male | 5 | 12 months | - |
| P4 | Male | 2 | 4 years | - |
| P5 | Female | 11 | 11 years | 19 years |
| P6 | Male | 4 | 5 months | - |
| P7 | Male | 8 | 2 years | 2 years 5 months |
| P8 | Male | 1 | 3 months | 6 months |
| Patients . | Sex . | Symptom onset (months) . | Age at diagnosis . | Current age . |
|---|---|---|---|---|
| P1 | Male | 6 | 2 years | - |
| P2 | Male | 2 | 6 months | - |
| P3 | Male | 5 | 12 months | - |
| P4 | Male | 2 | 4 years | - |
| P5 | Female | 11 | 11 years | 19 years |
| P6 | Male | 4 | 5 months | - |
| P7 | Male | 8 | 2 years | 2 years 5 months |
| P8 | Male | 1 | 3 months | 6 months |
Infectious agents and clinical manifestations
| Patients . | Infectious agents . | Viral serology . | Clinical manifestations . | Vital status . | Treatment . |
|---|---|---|---|---|---|
| P1 | Staphylococcus haemolyticus, Pseudomonas, Aspergillus | Not detected | Skin lesion, granuloma, pneumonia | Deceased | |
| P2 | Serratia marcescens | EBV IgM/IgG, CMV IgG | Pneumonia, abscesses, anemia | Deceased | |
| P3 | Salmonella sp. | CMV IgG | Abscesses, diarrhea, fever, anemia | Deceased | |
| P4 | Pseudomonas, Klebsiella, Candida | CMV IgG | Abscesses, diarrhea, fever, vomiting, pneumonia | Deceased | |
| P5 | Mycobacterium tuberculosis, Aspergillus | EBV IgG | Pneumonia, abscesses | Alive | ATB+ATF+Cortocoid |
| P6 | E. coli | CMV IgG, EBV IgG | Abscess, fever, diarrhea | Deceased | |
| P7 | Staphylococcus aureus | CMV IgG | Fever, cervical and axillary lymphadenopathy | Alive | TMP/SMX |
| P8 | No report | CMV IgM | Abscesses, pneumonia | Alive | TMP/SMX |
| Patients . | Infectious agents . | Viral serology . | Clinical manifestations . | Vital status . | Treatment . |
|---|---|---|---|---|---|
| P1 | Staphylococcus haemolyticus, Pseudomonas, Aspergillus | Not detected | Skin lesion, granuloma, pneumonia | Deceased | |
| P2 | Serratia marcescens | EBV IgM/IgG, CMV IgG | Pneumonia, abscesses, anemia | Deceased | |
| P3 | Salmonella sp. | CMV IgG | Abscesses, diarrhea, fever, anemia | Deceased | |
| P4 | Pseudomonas, Klebsiella, Candida | CMV IgG | Abscesses, diarrhea, fever, vomiting, pneumonia | Deceased | |
| P5 | Mycobacterium tuberculosis, Aspergillus | EBV IgG | Pneumonia, abscesses | Alive | ATB+ATF+Cortocoid |
| P6 | E. coli | CMV IgG, EBV IgG | Abscess, fever, diarrhea | Deceased | |
| P7 | Staphylococcus aureus | CMV IgG | Fever, cervical and axillary lymphadenopathy | Alive | TMP/SMX |
| P8 | No report | CMV IgM | Abscesses, pneumonia | Alive | TMP/SMX |
ATB = antibiotics, ATF = antifungals, TMP/SMX = trimethoprim/sulfamethoxazole, CST= corticosteroid treatment.
Laboratory findings
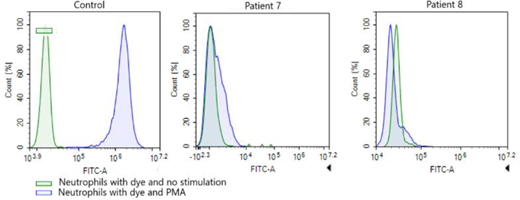
| Patients . | NBT1 . | DHR2 SI3 . | TB-PCR . | BCG-itis . | Affected gene . |
|---|---|---|---|---|---|
| P1 | 5 | Not done | Not done | No | CYBB |
| P2 | 5 | 1 | Not done | No | Not done |
| P3 | Not done | 2.4 | Not done | No | Not done |
| P4 | Not done | 2 | Not done | No | Not done |
| P5 | Not done | 1.5 | Positive | No | NCF2 |
| P6 | Not done | 1.2 | Not done | No | Not done |
| P7 | Not done | 1.1 | Negative | Yes | Not done |
| P8 | Not done | 0.9 | Not done | Yes | Not done |
| Patients . | NBT1 . | DHR2 SI3 . | TB-PCR . | BCG-itis . | Affected gene . |
|---|---|---|---|---|---|
| P1 | 5 | Not done | Not done | No | CYBB |
| P2 | 5 | 1 | Not done | No | Not done |
| P3 | Not done | 2.4 | Not done | No | Not done |
| P4 | Not done | 2 | Not done | No | Not done |
| P5 | Not done | 1.5 | Positive | No | NCF2 |
| P6 | Not done | 1.2 | Not done | No | Not done |
| P7 | Not done | 1.1 | Negative | Yes | Not done |
| P8 | Not done | 0.9 | Not done | Yes | Not done |
NBT: nitroblue tetrazolium.
DHR: 123 Dihydrorhodamine,
SI: stimulation index.
Dihydrorhodamine (DHR) test in patient 7, patient 8, and a healthy control.
The average age of diagnosis was 5 years. The mean diagnostic delay was 2 years and 5 months. Staphylococcus aureus, Pseudomonas spp., Aspergillus spp., and Salmonella spp. were the most frequently identified pathogens. The most common clinical manifestations were abscesses, pneumonia, and persistent fever. Less findings included skin involvement, lymphadenopathy, and gastrointestinal symptoms such as diarrhea and vomiting. Severe complications following Bacillus Calmette–Guérin vaccination occurred in two children.